Latest Updates
NEHEN reduces administrative burden through the adoption of standardized transactions. It is a cornerstone service for payer and provider trading partners wishing to exchange industry standard X12, HIPAA compliant transactions in a real-time, integrated manner using APIs. Because of our unique governance, non-profit status, and membership-based model, NEHEN is able to offer very competitive services relative to the market. Working with members and trading partners, NEHEN is also supporting a prototype electronic prior authorization (ePA) implementation that automates transactions using industry standard, open platform methods developed by the HL7 DaVinci Prior Authorization workgroup. Click HERE to learn more.
June 23, 2025
Through the first half of 2025, NEHEN sites collectively processed over 110 million transactions, with monthly volumes ranging from approximately 15.6 to 22.1 million. While activity dipped in March, volumes rebounded in April and May, reflecting steady engagement across the network. Several high-volume contributors consistently drove transaction counts, and new site activations helped offset any terminations. BCBSMA, Medicaid, Medicare, and United Healthcare were the top transaction recipients during the first half of the year, with eligibility and benefits (270/271) and claims (837) contributing to most of the overall volume, while referrals (278) and claim status inquiries (276/277) showed steady but lower usage. Initial June transaction volumes signal continued demand for NEHEN’s connectivity and administrative data exchange services. Email NEHEN@mahealthdata.org for more information.
December 11, 2024
As many of you know, we have been working to support the interoperability and prior authorization requirements specified in the CMS-0057F rule (among others). These regulations outline how payers and providers must exchange detailed clinical and administrative data to enable real-time prior authorizations as well as patient, provider, and payer access to administrative, clinical, and other health data. In addition, we are providing exchange services related to quality measures to the community as the next step in the existing quality measures programs in our Data Governance Collaborative.
These new use cases incorporate HL7® FHIR® standards via API (Application Programming Interface) endpoints, enabling future interoperability and integration opportunities. The timeline for payers and providers to adopt these defined transactions is January 1, 2027.
Services for these use cases are available in two models:
- Passthrough Exchange Services (supports prior authorization and quality measures): Used by all participants, these services use the foundational Core FHIR platform to exchange data directly between NEHEN participants
- Optional Hosted Services (supports all FHIR-based services): Available for health plans and (in some cases) providers, these services are handled by directly by NEHEN on behalf of the intended recipient (for example, NEHEN might respond directly to requests asking if a particular procedure needs a prior authorization for a patient covered by a specific payer plan)
We are finalizing an agreement with ZeOmega to be our primary FHIR vendor for the bulk of these capabilities, with implementations slated to start in early 2025.
These new FHIR services will augment and integrate with our existing X12 EDI services, not replace them, providing an expanded suite of features and capabilities. We are excited about the potential these services offer our participants and look forward to collaborating with all of you in the months ahead.
April 15, 2024
MHDC is offering support for providers and payers affected by the Change Healthcare cyberattack on Feb 21, 2024. This unprecedented outage has affected operations and finances of thousands of payers and providers. TriZetto and the NEHEN team immediately disconnected NEHEN from Change Healthcare’s network as a precautionary measure and to ensure NEHEN users were insulated from the attack. Since the outage started, we have been working with TriZetto to reroute payer connections that relied on the Change Healthcare network to retain and support operational resiliency.
The impact of this incident highlights the vulnerability of relying on a single solution for access to trading partner EDI transactions such as claims, eligibility, remittance advice, and referrals. NEHEN users are fortunate to have been minimally impacted by this outage because we maintain direct connections to our payers and providers (to avoid exactly this type of exposure). We also maintain secondary (redundant) connections to our payers. MHDC is advocating for industry response requiring single source clearinghouse services to maintain similar alternate routes and redundancy of capabilities for their networks in the future.
Meanwhile, the NEHEN team has been providing a number of support services for the impacted providers and payers under MHDC's Change Healthcare Assistance Program (CHAP), sponsored by the Mass Collaborative. CHAP includes a rapid onboarding service to NEHEN EDI exchange for providers seeking alternative claims submission and remittance processing options. Visit the CHAP website for more details including links to resources and tips on selecting an EDI service organization. MHDC is holding open office hours via Zoom weekly on Thursdays at 12:00 (Register Here). These are open to all to share resources, discuss options people are using to mitigate the impact of this extended outage, and learn more about the CHAP program.
December 14, 2023
As noted in our Executive Director’s message at the start of this newsletter (Winter 2023/2024 issue), the NEHEN 3.0 RFP process is well underway, However, NEHEN’s current support will not change for the foreseeable future. The next two years will be spent preparing for the uptake and adoption of new prior authorization and quality measure rules and early integration/testing of these services prior to widespread adoption at the beginning of 2026 (some quality measure requirements start during 2025). We are expecting the final rule covering prior authorization by mid-January and proposals for the provider side regulations and related EHR certification processes from ONC as soon as later this month. We anticipate the NEHEN 3.0 timing to align well with regulatory deadlines.
The NEHEN 3.0 deployment process will be iterative and adaptive to shifts in requirements, standards, and the needs of our members. We have built this type of agile approach into the RFP and have made it a central component of our NEHEN 3.0 plans. We look forward to embarking on this journey with all of NEHEN and the larger MHDC community!
Aside from the work going on with NEHEN 3.0, NEHEN recently renegotiated an extension to our services agreement with Cognizant/TriZetto (TPS). This new agreement will allow for re-tooling of our current arrangement with TPS to accommodate the plans we have underway for new API and FHIR based services described in the NEHEN 3.0 RFP.
The new agreement allows NEHEN participants to benefit from extended services offered by TPS for both payers and providers such as:
Payer Features:
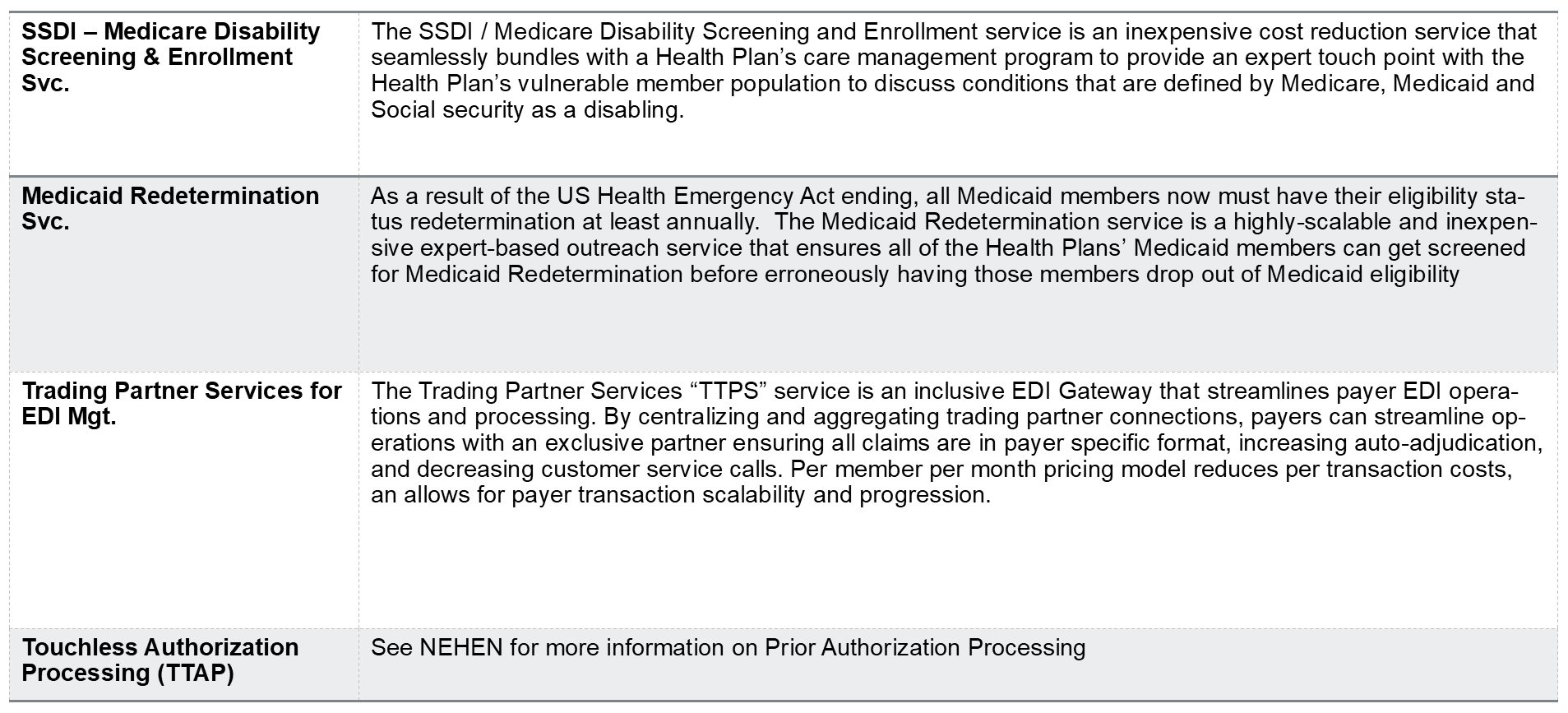
Provider Features:
.png?width=1538&height=740&name=image003%20(1).png)
July 12, 2023
As of June 21, most Point32Health systems are back online, including the member, employer, and broker portals as well as enrollment, claims, and billing systems. All Harvard Pilgrim Health Care and Tufts Health Plan NEHEN transactions have returned to normal processing. There is a backlog of manual transaction processing to catch up on which will take some time. Current systems may reflect their mid-April statuses until this is complete. On behalf of Point32Health, we thank our NEHEN users for their patience, support, and flexibility during this challenge.
As outlined in the NEHI final report referenced in last month’s newsletter, there is a compelling case for a statewide coordinated effort regarding electronic prior authorization. MHDC and NEHEN have recently met with several industry groups and various stakeholders to discuss plans in this area including standardization and coordinated onboarding processes.
In these meetings (with the Massachusetts Association of Health Plans, the Blue Cross Blue Shield Clinical Advisory Board, and others), we have heard directly from payers and providers about their concerns with electronic prior authorization. They have universally supported taking a centralized, coordinated approach. MHDC will create a Technical Assistance Center to support implementation. We have asked for state funding to help defray participant costs but no commitment has been made at this time.
MHDC is working on an RFP for what we’ve been calling NEHEN 3.0 which incorporates support for electronic prior authorization transactions as part of a coordinated effort to advance NEHEN’s technology and services. The full plan involves improving NEHEN’s current X12 EDI services, standing up core FHIR API exchange services, and supporting ePA and two other high priority data exchange use cases (quality measures and equity). We’re calling this initial set of functionality phase 1. We intend to build this initial system with the capacity to add on additional use cases in the future; we’ve already identified some potential phase 2 functionality (including CMS-mandated payer and provider exchanges like the payer=>payer API and Provider Access API in the latest CMS proposed interoperability rule among others). However, we are not planning to identify specific phase 2 plans now.
Our approach to the entire project will be iterative and we plan to leverage knowledge gained during the initial efforts to guide how we move forward. The RFP outlining the NEHEN 3.0 plans in more detail and soliciting vendors for phase 1 should be released later this summer. Feel free to contact us at rfp@mahealthdata.org if you have any questions about the RFP or would like to be notified when it's released.
June 1, 2023
Last month’s newsletter described the cyberattack events on April 17 that required Point32Health (Tufts Health Plan and Harvard Pilgrim Healthcare) to shut down their IT services for the protection of member and plan data. After extensive remediation and forensic analysis Point32 was able to bring the Tufts Health Plan systems back online on April 27th. However the Harvard Pilgrim systems still remain partly unavailable.
We were able to safely resume eligibility verification services for Harvard Pilgrim via NEHEN for both the integrated node transactions and portal activity on May 23rd. Services that remain unavailable are new claims submissions (837), remittances (835), claims status inquiries (276/277) and referrals (278). Claims that were submitted prior to the attack have been paid or are in the process of being paid. We will continue working with Point32Health on the safe and secure return to full normal operations as the remediation and validation work allows. Please refer any questions or concerns to the Point32Health provider and patient support lines. Additional information can be found HERE. We thank all of our members for their patience and support during this challenging time. Together we are all stronger in support against cyber crime.
Meanwhile NEHEN has been very engaged with the work of the NEHI and MHDC ePA initiatives. We completed and released the final report of the ePA Automation Advisory Group (TAAG) which can be read in its entirety HERE. We encourage all payers and providers in Massachusetts to read this report on the recommendations of the group and insight into our proposed direction for a statewide coordinated effort to rapidly advance ePA in Massachusetts over the next two years. The recommended approach is aligned with the CMS proposed rule for ePA but adds additional guidance, clarifications, and requirements.
We capped the work of the TAAG with a presentation to the Health Policy Commission (HPC) on May 10th where we received positive feedback on the final report and the recommendations. The HPC will be taking up the topic further at the HPC board meeting this month. Recommendations they’re considering from the report include a statewide Technical Assistance Center (TAC) to help payers and providers acquire technical solutions and implement them and formation of a multi-stakeholder task force to provide governance and oversight of the overall use of prior authorization and how it’s meeting goals of improving care while managing cost. Having this task force look at clinical evidence and outcomes, usage patterns, and other relevant data and metrics with an eye toward how it’s working and any needed adjustments is an essential part of implementing an ePA program and ensuring it meets the stated goals.
According to Bob Dieterle of EnableCare and DaVinci, the volume of real-time transactions in a fully implemented ePA world will likely surpass the current EDI (traditional HIPAA mandated X12 messages) by an order of magnitude (at least 10x the volume). Having a robust infrastructure and scalable capability to handle this traffic is essential to success. MHDC and NEHEN are working on this for Massachusetts and possibly beyond. We see ePA as the start of the next big evolution in healthcare as it combines real-time exchange of both clinical and administrative data between payers, providers, and patients. Come join us on this exciting journey.
May 1, 2023
We recently received a stark reminder that no one is immune from cyberattacks with the news about a successful attack on our largest NEHEN payer, Point32Health (Point32Health combines Tufts Health Plan (THP) and Harvard Pilgrim Health Care (HPHC) into a single entity). At the time of this writing, NEHEN is working closely with Point32Health and our technical services provider, Cognizant/TriZetto, to bring services back online for members. However we have no firm estimates of the timeline to make that happen; the timing may be different for requests going to THP and HPHC.It is often said the it’s not a matter of if you will experience a breach or attack but when and what it will be. As we provide the support we can to Point32Health, this should serve as a reminder to us all to be continually diligent about activity on our networks that could be used to compromise systems, infrastructure, or operations.
We are continuing to work on moving NEHEN toward the future. There are currently three dimensions to these efforts:
- Making existing EDI services more cost efficient and effective
- Offering FHIR API services for the exchange of key clinical and administrative data between payers and providers
- Standing up prior authorization services starting with Coverage Requirements Discovery (CRD)
We also anticipate continuing our ongoing efforts to improve and standardize electronic prior authorization in conjunction with local stakeholders and organizations like NEHI and the Health Policy Commission (HPC), wrapping up the first phase of the project over the next two months. As part of this work, NEHI just released our joint Advanced Prior Authorization Automation Across Massachusetts report. Our final TAAG meeting was held on Tuesday April 25th which will be followed by publication of our final report in May after review by the HPC. There will also be a public webinar on May 24th - see the MHDC Events section for more information and registration details.
April 3, 2023
On the ePA front, we continue to work with the Network for Excellence in Healthcare Innovation (NEHI) and the Health Policy Commission (HPC) on a statewide plan for adopting fully automated electronic prior authorization by 1/1/2026, using the three DaVinci implementation guides (IGs) covering the prior authorization process.
We recently provided the HPC with a draft of the final report of the work we have been doing over the past 6 months including input from the TAAG (Automation Advisory Group) and meetings and interviews with industry stakeholders including payers, providers, vendors, regulators, CMS, ONC, and other policy makers. This report includes a set of recommendations including:
- Formation of a task force to guide the coordination of prior authorization adoption in Massachusetts
- A project plan for automating prior authorization
- Creation of a technical assistance center
- Creation of a state designated point of oversight for reporting and governance.
There will be a final meeting of the TAAG group to review the recommendations after the HPC comments on the report. We meet with the commissioners on May 10th to present it for their consideration. Once the report is finalized, we will also hold a public webinar to present the work we’ve done, our recommendations, and the plan going forward. Watch this space and our social media for more information.
Point of Care Partners (POCP) has made some initial recommendations of potential future FHIR-based services for NEHEN based on their stakeholder interviews discussed in our March update. The potential services recommended for consideration include API gateway services and acting as an intermediary to assist with translations between FHIR and X12 (for those services requiring them). We are evaluating different models of facilitated FHIR exchange across multiple use cases including possibly the Provider Access APIs, Payer => Payer APIs, and prior authorization-related APIs as well as others.
Our board subcommittee will meet and review these recommendations, discuss the model for delivery, and decide on a course moving forward. Watch this space for more information about future plans after that discussion is complete. We believe these services could greatly enhance the NEHEN experience for our users.
March 1, 2023
NEHEN is working with Point-of-Care Partners (POCP), the industry group who supports and runs the program office for the DaVinci and other FHIR accelerators, to gather feedback and stakeholder input on potential services and use cases that NEHEN could support in the future. We will reconvene a designated sub-committee of our Board to review the initial recommendations from POCP followed by a process to start planning implementation of some or all of the approved recommendations.
This is necessary because the standards and methods of exchanging administrative and clinical data are changing. This is clear from ongoing CMS regulatory actions as well as many other industry signals. API-based exchange services will be the norm for both administrative and clinical data in the not-too-distant future; there is no desire for advancing traditional EDI services. As part of this transition, the industry is looking to converge traditional EDI transactions and standards (X12) with existing document-based standards (C-CDA) and API-based standards (FHIR) using JSON and/or XML for their data.
There has been some industry feedback (by HL7 and others) that the use of the C-CDA standard for attachments, as proposed in the attachments proposed rule, is an outdated approach; there are FHIR equivalents which better accommodate clinical and other needed data. CMS argues this may be true but the C-CDA standard is widely used standard today while FHIR is still emerging with significantly less current adoption. We feel that as long as regulations remain adaptable to new and emerging standards it is more important to get an attachment rule in place as soon as possible than to quibble over its format requirements. We believe the C-CDA standard is more specifically aligned with provider => provider exchanges, particularly those using HIEs and TEFCA/QHINs (where C-CDA is the expected norm). However, it does accommodate other use cases and allows for other types of attachment data like FHIR resources, images, and more. We hope as FHIR becomes more commonplace the attachment rule will be adjusted to permit direct FHIR exchange and not just FHIR-formatted data.
On the ePA front, the prototype of the CRD (Coverage Requirements Discovery) implementation between Blue Cross Blue Shield of Massachusetts (BCBSMA) and New England Baptist Hospital (NEBH) is complete. We have collected the data and content needed to publish an industry report on the results; this report is pending and should be available soon. We were successful in setting up a DaVinci-compliant CRD service within the NEBH environment, hosted by Olive, to validate and demonstrate the viability of a production-ready, CDS Hooks-compliant service request-response mechanism. We were encouraged by the results of this prototype and continue to believe that there is great value for both payers and providers in the CRD process alone and even more in the entire prior authorization workflow.
Meanwhile, MHDC and the Network for Excellence in Healthcare Innovation (NEHI) have formulated a set of recommendations for the Health Policy Commission (HPC) to consider for the support and advancement of electronic prior authorization adoption statewide. Why is this still necessary now that there’s a CMS proposed rule covering this process (and more)? In part because the CMS rule does not apply to all payers or all plans and because it does not require the use of the DaVinci implementation guides which are important for more standardization and consistency in implementations. The Automation Advisory Group providing oversight on this project also felt that a centralized coordinating function with accompanying adoption support would greatly improve the consistency, quality, and results from resulting prior authorization implementations.
The planned presentation of recommendations to HPC was delayed and we are working on rescheduling it now. We’ll report on state-based plans further when more information is available.
February 1, 2023
To quote the Workgroup for Electronic Data Interchange (WEDI), "It’s Raining Regulations." NEHEN called the latter part of 2022 "the Season of Letters." Either way you look at it, this has been an unprecedented period of activity on the standards and regulatory front, with more to come.
As expected, the Advancing Interoperability and Improving Prior Authorization Processes Proposed Rule was released on December 13, 2022 with a 90 day public comment period (ending on March 13, 2023) and an effective date of January 1, 2026 for all of the included components. It builds on the May 2020 Interoperability and Patient Access rule by adding additional requirements to the Patient Access API, mandating that the Payer => Payer exchange happen via FHIR and support bulk requests around enrollment periods, that a new Provider Access API be stood up to support payer exchange of administrative and clinical data with providers, introduced a new real time prior authorization workflow using FHIR APIs and other technology, and a few other smaller items (see our feature article for more details).
In addition, HHS published an attachments proposed rule on December 21, 2022. The industry has been waiting for this rule for a long time to support sending of attachments with information needed for efficient processing of claims, referrals, and prior authorization requests to payers. This rule supports the Interoperability and Prior Authorization proposed rule discussed above, particularly as the recommended DaVinci prior authorization IGs reference the X12 275 standard for exchange of FHIR bundles and in support of Request for Additional Information transactions between the payer and provider. The standard proposed for attachments is the HL7 CDA R2 (with support for data in other formats - such as FHIR - within the transaction). This standard was chosen based on a July 15th, 2016 letter from National Committee on Vital Health Statistics (NCVHS) to the Secretary of HHS, HERE. There are also proposed operating rules developed by CAQH CORE for attachments which have not yet been recommended to CMS by NCVHS. The proposed rule has a two year compliance timeframe right now, with actual date selection pending finalization of the rule.
Additionally, we participated in a two day NCVHS Subcommittee Hearing in January that presented these proposed standards and operating rules and collected industry feedback on their proposed adoption. Day 1 covered version 8020 of the X12 standards for claims and remittances and day 2 focused on a panel of proposed operating rules from CAQH CORE in support of infrastructure, connectivity, patient attribution, and attachments rules. MHDC generally supports the adoption of these proposed rules. There is clearly an opportunity for the regulators to coordinate, collaborate, and converge on the development, use, adoption, and deployment of regulatory standards in a cadence and predictable schedule that would create a more cohesive and predictable coordination of standards adoption going forward.
NEHEN has been working closely with the Network for Excellence in Healthcare Innovation (NEHI) on a framework to advance adoption of automated electronic prior authorization in Massachusetts for consideration by the Health Policy Commission (HPC). The third meeting of The Automation Advisory Group working on this was held on December 22, 2022 with stakeholders from the HPC, CMS, ONC, EOHHS, NEHI, NEHEN, MHDC, and MHA as well as from health plans, providers, and vendors in attendance. We discussed what we plan to accomplish and how to accomplish it, including adaptation of the DaVinci prior authorization IGs to address more flexible workflow options for payers and providers as well as clarification of specific data formats and data content requirements to better meet the needs of our stakeholders. We will be meeting with the commissioners on the board of the HPC on Feb 15th, 2023 to present these recommendations and chart a path forward.
December 15, 2022
NEHEN is working on a strategic plan for 2023 and beyond. We hope to support a set of new services evolving toward integrated and converged transactions leveraging FHIR and other modern technologies. MHDC has engaged Point of Care Partners (the folks who staff the DaVinci and other FHIR accelerator PMO roles) and formed a committee of our Board of Directors and other stakeholders to determine the best services to support and a related roadmap going forward.
Speaking of DaVinci, our DaVinci compliant Coverage Requirements Discovery prototype service between Blue Cross Blue Shield of Massachusetts and New England Baptist Hospital was scheduled to go live on December 10, 2022 (still waiting on final confirmation). We will closely monitor the transactions - expect reports in future NEHEN updates.
In industry news, the pending CMS Prior Authorization rule has cleared the Office of Management and Budget, typically the last step in the process before release of a new regulatory rule, and could be released at any times (it's possible it came out between our writing this update and the actual newsletter release). It should be released as a proposed rule with a public comment period before the rule is finalized. It is also unclear whether the rule will include the non-prior authorization components that were part of the original frozen rule or just be focused explicitly on prior authorization. Either way, it will have a major impact on ePA adoption throughout the industry.
Meanwhile, NCVHS is in the process of reviewing the CAQH Core and X12 HIPAA advancement requests discussed in last month's update. CAQH Core has a new website where you can see the proposed new operating rules with a side-by-side comparison to the existing rules as well as other information. Among other things, these rules include advancements to support prior authorization including the addition of an indication whether prior authorization is required within 270/271 Eligibility and Benefits transactions and support for attachments to send clinical and other data as FHIR resources or in other formats.
With these and other new rules, we continue to see convergence of the existing administrative data rules with advancements in clinical data exchange and other transactions moving beyond traditional X12 EDI processes. This convergence is needed for the industry to move forward cohesively and in a coordinated manner. Efficiency, transparency, access, equity, quality, and other operational and business imperatives all depend on having a clear roadmap for using all of the standards and rules together effectively. The more standardized processes, interfaces, and data are the better we all operate and the more resources we can devote to initiatives that move us forward and benefit everyone - payers, providers, and patients alike.